
 In recent decades, all regions of the world have seen substantial progress in life expectancy at birth, which was estimated to be at 72.8 years in 2019 compared with 64.2 years three decades ago. As importantly, life expectancy has increased at all ages such that a person at age 65 in 2019 was likely to live 6.2 years longer than in the early 1950s (United Nations, 2022). But life expectancy differs significantly across countries and within them. Inequalities in health and in life expectancy across countries have received attention from the international community, which recognized that such inequalities are unfair and beyond an individual’s control. Assessing country-level inequality in life expectancy is therefore useful to examine whether outcomes in countries with high increases in life expectancy differ by their social and health policies. For instance, reducing inequality in life expectancy across countries points to the role that health policies play in controlling a wide range of diseases responsible for disparities in child and maternal mortality.
In recent decades, all regions of the world have seen substantial progress in life expectancy at birth, which was estimated to be at 72.8 years in 2019 compared with 64.2 years three decades ago. As importantly, life expectancy has increased at all ages such that a person at age 65 in 2019 was likely to live 6.2 years longer than in the early 1950s (United Nations, 2022). But life expectancy differs significantly across countries and within them. Inequalities in health and in life expectancy across countries have received attention from the international community, which recognized that such inequalities are unfair and beyond an individual’s control. Assessing country-level inequality in life expectancy is therefore useful to examine whether outcomes in countries with high increases in life expectancy differ by their social and health policies. For instance, reducing inequality in life expectancy across countries points to the role that health policies play in controlling a wide range of diseases responsible for disparities in child and maternal mortality.
Capturing variation in ages at death within countries matters
There is a growing interest in assessing inequality in life expectancy within countries, its evolution over time and its key determinants. In many countries with data, evidence points to the importance of socioeconomic status (usually proxied by income, education or occupation) as a key determinant of inequality in life expectancy. Inequality in life expectancy driven by income differences can manifest in different ways, including through access and utilization of health care. Cost barriers could lead to unequal access to and utilization of health care, differing adoption of technological innovations in medicine and preventive health behaviors. Those with higher socioeconomic status have greater access to the resources needed to receive better and earlier medical care in order to avoid disease or minimize its impact (Braveman, Egerter and Williams, 2011). A worrisome trend observed in some developed countries with data is that socioeconomic disparities in life expectancy have increased over time. For instance, a comparative analysis between the United States and Denmark shows that from 2001 to 2014, individuals in the highest income terciles gained more years of life expectancy than the poorest and had higher chances of surviving into older ages in both countries (Dahl and others, 2021). Additional studies in the United States find that larger increases in life expectancy were seen among those with higher socioeconomic status and stagnation or decrease in life expectancy were experienced among the lowest socioeconomic group (Bor, Cohen and Galea, 2017). While midlife mortality declined among high socioeconomic groups, it decreased less rapidly and sometimes increased among low socioeconomic groups more exposed to environmental and occupational hazards. This implies that midlife mortality rates, if suitably targeted and addressed, have the potential of drastically reducing lifespan inequality. Monitoring lifespan variation would have informed the midlife mortality crisis that confronts the United States since 2014 (van Raalt, Sasson and Martikainen, 2018). Inequality in life expectancy by income is not uniform among men and women. In Norway, for instance, women in the top one per cent of the income distribution can be expected to live 8.6 years longer than women in the lowest one per cent. For men, the difference in life expectancy at birth between the top one per cent income earners and the bottom one per cent is 13.8 years (Kinge and others, 2019). A study of 15 European countries, using level of education as a measure of socioeconomic status, revealed considerable gaps in life expectancy at birth, but the results varied between countries, with a 2.1-year difference between the highest and lowest educated men in Spain and more than an 8-year difference between these groups in Lithuania. The gaps were smaller for women, but still persistent. Women in Spain had a 0.6-year difference in life expectancy at birth while women in Lithuania saw a gap of more than 4 years between the highest and lowest educated groups (Mackenbach and others, 2019). Between 1990 and 2018, college educated adults in the United States were likely to live more than three years longer than those without a degree, and reach an average age of 73.2. This educational divide was present for college educated Black and White people. Over this period, between those with and without a college education, the racial divide narrowed by 70 per cent and the educational divide doubled (Case and Deaton, 2021). 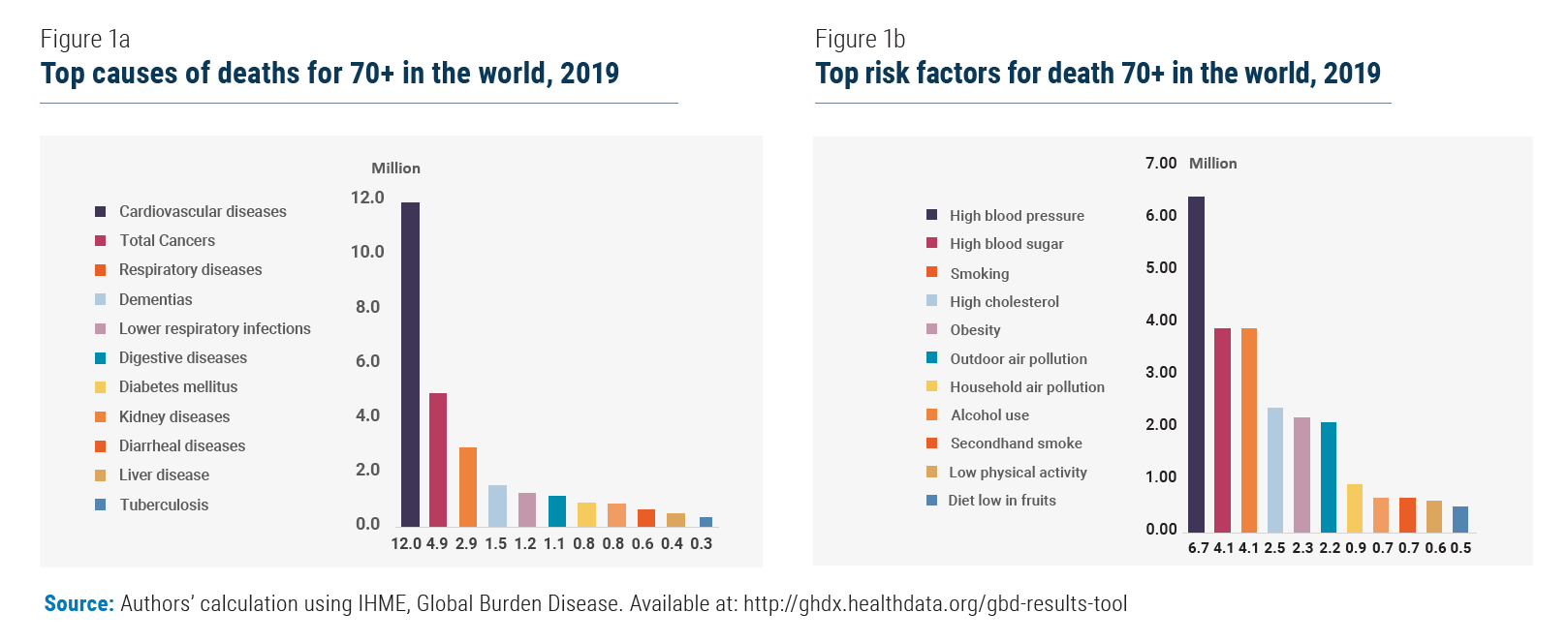
Disparities in life expectancy are moving to later stages in life
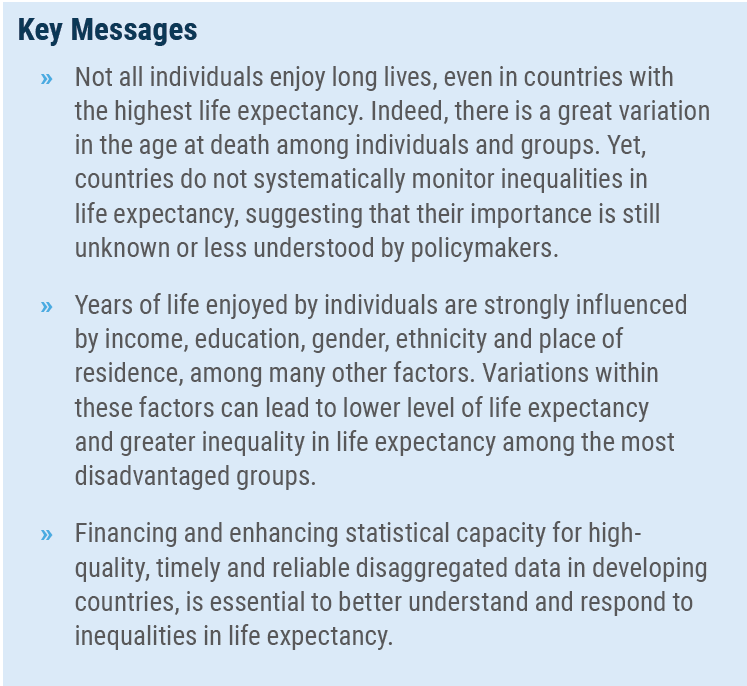
As a result of reduced child mortality rates, increased living standards and medical progress, there has been a shift in mortality disparities from early to later life leading to life expectancy inequality among older persons. Worldwide, about two-thirds of the deaths are estimated to take place at age 60 and older while almost half of all the deaths occur at age 70 and above in 2021 (United Nations, 2022). Understanding causes of death among older persons and identifying risk factors associated with these causes can help to partially explain inequality in life expectancy among older persons. On the one hand, most deaths in the over-70s age bracket are caused by non-communicable diseases (NCD) such as cardiovascular diseases, cancers, dementia, diabetes and chronic respiratory diseases (figure 1a). Socioeconomic inequality in mortality has played a role in the United States because cardiovascular death rates decreased more slowly in lower than in higher socioeconomic groups (Jemal and others, 2008). On the other hand, the leading risk factors associated with death among older persons are high blood pressure, high blood sugar (hyperglycemia), smoking and obesity (figure 1.b). Gender disparities in life expectancy among older persons partially reflect different exposure to risk factors such as tobacco and alcohol use, along with unhealthy diets. For example, in many developed countries, men are more likely to die from cancer, heart and other diseases after the age of 65, while women often experience higher rates of chronic conditions that are less likely to result in early death such as arthritis and depression (Carmel, 2019). The rapid increase in life expectancy at all ages has raised the question on the number of extra years spent in good health particularly among older persons which represent the segment of the population suffering most from higher disability rates. As life expectancy has increased among older persons, healthy life expectancy has also increased although less rapidly and with differences across regions. Figure 2 shows that Europe had the highest healthy life expectancy at old age followed by the Americas, while the African region trails behind other regions. 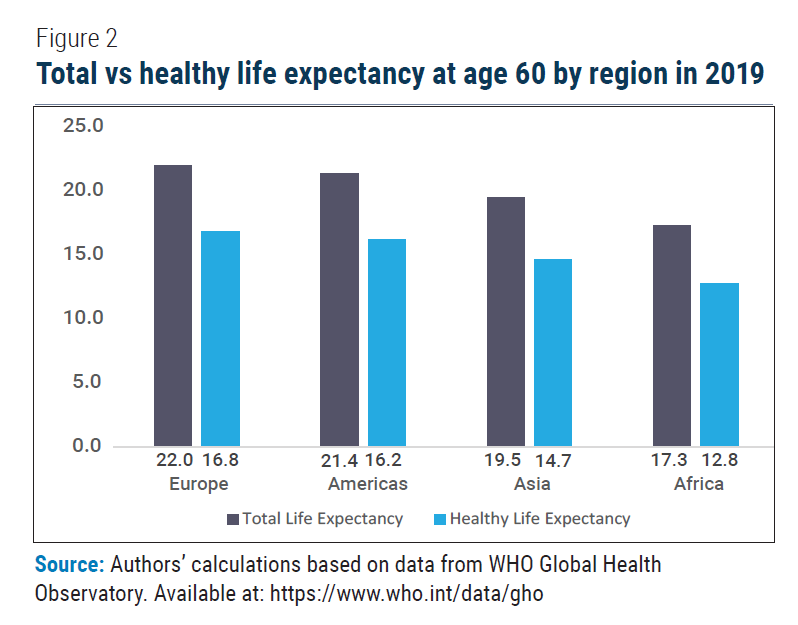 The difference between total and healthy life expectancy across regions is an indication of the number of years in which people live with a given disease burden or disability. The incidence of disability increases with age as physical and cognitive functioning tend to decline as people grow older. On average, healthy life expectancy at age 60 is five years shorter than life expectancy at age 60. In other words, older persons are likely to spend 25 per cent of their life after the age of 60 in illness or with injury. The impact that higher disability rates have on life expectancy inequality depends on the degree, amongst other factors, to which people with disabilities benefit from social protection transfers and health care services. Healthcare expenditure plays a pivotal role in this. Compared to low-income countries, healthcare expenditure (per capita or as the share of GDP) tends to be much larger in high-income countries, with a positive impact on new medical treatments, healthcare insurance coverage and access by disadvantaged groups to health care services. However, it is important to note that increased healthcare expenditure does not necessarily translate into wider insurance coverage and better access to health care services. The United States, for instance, is one such example. The rapid increase in healthcare expenditure is driven by significant improvements in medical treatments while total health insurance coverage remained stable for decades. As a result, healthcare expenditure in the country is highly concentrated amongst the top 5 per cent of spenders accounting for half of personal healthcare spending. That is the reason why early-life interventions seeking to promote healthy ageing are also central. These prevention policies would also have beneficial effects on the economy by allowing substantial savings of health expenditures.
The difference between total and healthy life expectancy across regions is an indication of the number of years in which people live with a given disease burden or disability. The incidence of disability increases with age as physical and cognitive functioning tend to decline as people grow older. On average, healthy life expectancy at age 60 is five years shorter than life expectancy at age 60. In other words, older persons are likely to spend 25 per cent of their life after the age of 60 in illness or with injury. The impact that higher disability rates have on life expectancy inequality depends on the degree, amongst other factors, to which people with disabilities benefit from social protection transfers and health care services. Healthcare expenditure plays a pivotal role in this. Compared to low-income countries, healthcare expenditure (per capita or as the share of GDP) tends to be much larger in high-income countries, with a positive impact on new medical treatments, healthcare insurance coverage and access by disadvantaged groups to health care services. However, it is important to note that increased healthcare expenditure does not necessarily translate into wider insurance coverage and better access to health care services. The United States, for instance, is one such example. The rapid increase in healthcare expenditure is driven by significant improvements in medical treatments while total health insurance coverage remained stable for decades. As a result, healthcare expenditure in the country is highly concentrated amongst the top 5 per cent of spenders accounting for half of personal healthcare spending. That is the reason why early-life interventions seeking to promote healthy ageing are also central. These prevention policies would also have beneficial effects on the economy by allowing substantial savings of health expenditures.
Increased understanding of inequality in life expectancy is essential to guide policymakers
Monitoring inequality in life expectancy provides important insights about disparities in health and mortality. Socioeconomic status has been recognized as a key determinant of inequality in life expectancy. As such, increasing life expectancy for all socioeconomic groups to match the rate of the highest socioeconomic group is a way for countries to reduce inequality in life expectancy and ensure that rising life expectancy is of benefit to all individuals regardless of their age and other socioeconomic attributes. There are many mechanisms through which socioeconomic status creates inequality in life expectancy. The importance of these mechanisms such as health behaviours, access to and utilization of health care vary across countries and over time. Identifying factors contributing most to inequality in life expectancy is an important objective for determining appropriate policies. Lack of data challenges the analysis of the socioeconomic determinants of lifespan inequalities in many developing countries. Enhancing financing and statistical capacity for high-quality, timely and reliable disaggregated data in developing countries is therefore essential. Inequality in life expectancy prevailing among older persons and lower socioeconomic groups also has important implications for pensions. Inequality in life expectancy can have a considerable bearing on the length of retirement, running a risk that disadvantaged groups receive less pension as they tend to die earlier. Relatedly, reforms aimed to extend the economic activity and the productivity of the older population by increasing retirement age can be seen as a regressive measure if they do not account for inequality in life expectancy.
 Welcome to the United Nations
Welcome to the United Nations


