 People in almost all countries are living longer. Globally, babies born in 2022 are expected to live 71.7 years on average, 25 years longer than those born in 1950. Rapidly ageing populations have increasing health and long-term care needs. As the forthcoming World Social Report 2023 discusses, however, today’s care and support systems for older persons are insufficient, requiring greater policy attention. The Covid-19 pandemic exposed existing weaknesses across countries in approaches to long-term care and showed how these weaknesses can aggravate inequalities. Poor quality and underfunded care facilities, insufficient provisions for care at home, low wages and precarious working conditions for paid care workers all contributed to increasing the already significant threat of Covid-19 for older persons (United Nations, 2020). The speed of change and the scale of the crisis have strengthened the call for fundamental reform of approaches to long-term care. Failure to do so will harm today’s older persons and those who care for them, as well as future generations of older persons.
People in almost all countries are living longer. Globally, babies born in 2022 are expected to live 71.7 years on average, 25 years longer than those born in 1950. Rapidly ageing populations have increasing health and long-term care needs. As the forthcoming World Social Report 2023 discusses, however, today’s care and support systems for older persons are insufficient, requiring greater policy attention. The Covid-19 pandemic exposed existing weaknesses across countries in approaches to long-term care and showed how these weaknesses can aggravate inequalities. Poor quality and underfunded care facilities, insufficient provisions for care at home, low wages and precarious working conditions for paid care workers all contributed to increasing the already significant threat of Covid-19 for older persons (United Nations, 2020). The speed of change and the scale of the crisis have strengthened the call for fundamental reform of approaches to long-term care. Failure to do so will harm today’s older persons and those who care for them, as well as future generations of older persons.
Long-term care provision falls disproportionately on women
Traditionally the care needs of older persons have been met—for better or worse—within co-habiting extended families and most often by the female members of those families, including older women. However, in more developed countries in particular, intergenerational co-residence has declined dramatically in recent decades. Most older persons in these countries live either in single-person households or in households consisting of a couple only or a couple and their unmarried children. These changes in living arrangements have contributed to an increasing demand for long-term care (United Nations, 2019). Because, on average, they live longer and spend a longer period of their lives in poor health, older women are more likely to need long-term care services compared with older men. Women are also usually frailer and have worse health at the end of life than men (Hägg and Jylhävä, 2021). As a result, older women tend to account for a higher proportion of care recipients compared to older men. In the European Union, at ages 65 and over, 33 per cent of women needed long-term care compared with 19 per cent of men (European Union, 2021). Also, because women live on average longer than men and the common practice of women marrying men that are older than them, a larger proportion of older women are widows and lack direct support from a spouse. 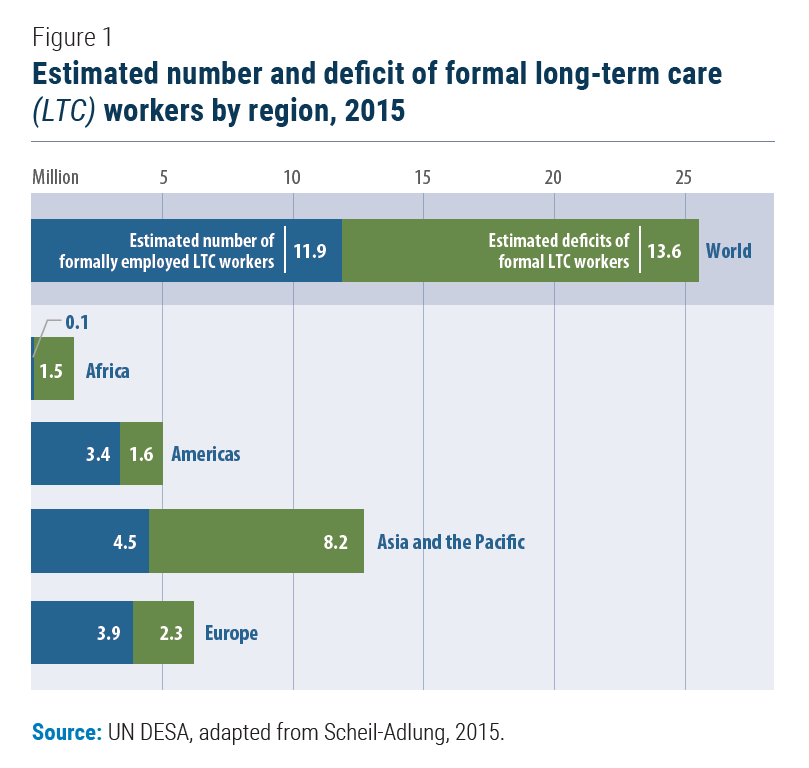 However, the supply of caregivers is not keeping pace with increasing demand. One study put the deficit at 13.6 million formal long-term care workers (Scheil-Adlung, 2015) (see Figure 1). Foreign-born migrants have often filled gaps in supply of care workers. In Italy, for instance, an estimated 73 per cent of the paid care workforce in 2017 was foreign-born (Bonizzoni, 2019). Migrant care workers are often in an irregular situation and therefore can only work in the informal economy, with limited protection and low wages. Many countries, even high-income ones, will continue to rely on informal care provision. In Europe, for instance, estimates suggest that as much as 80 per cent of all long-term care is provided by informal care givers, and that the number of informal caregivers ranges from 10 up to 25 per cent of the total population (European Commission, 2018). Most caregivers—both paid and unpaid, in formal and informal sectors—are women. This is a common phenomenon across regions and across countries of different income levels. Globally, women spend an average of over 50 minutes per day on unpaid care work—such as taking care of children and older persons—more than double the time spent by men. Nine in ten formal long-term care workers in OECD countries are women. Even in countries which have achieved the greatest gender equality, such as Denmark and Norway, the proportion of formal care workers who are women is 95 per cent and 92 per cent, respectively (OECD, 2021).
However, the supply of caregivers is not keeping pace with increasing demand. One study put the deficit at 13.6 million formal long-term care workers (Scheil-Adlung, 2015) (see Figure 1). Foreign-born migrants have often filled gaps in supply of care workers. In Italy, for instance, an estimated 73 per cent of the paid care workforce in 2017 was foreign-born (Bonizzoni, 2019). Migrant care workers are often in an irregular situation and therefore can only work in the informal economy, with limited protection and low wages. Many countries, even high-income ones, will continue to rely on informal care provision. In Europe, for instance, estimates suggest that as much as 80 per cent of all long-term care is provided by informal care givers, and that the number of informal caregivers ranges from 10 up to 25 per cent of the total population (European Commission, 2018). Most caregivers—both paid and unpaid, in formal and informal sectors—are women. This is a common phenomenon across regions and across countries of different income levels. Globally, women spend an average of over 50 minutes per day on unpaid care work—such as taking care of children and older persons—more than double the time spent by men. Nine in ten formal long-term care workers in OECD countries are women. Even in countries which have achieved the greatest gender equality, such as Denmark and Norway, the proportion of formal care workers who are women is 95 per cent and 92 per cent, respectively (OECD, 2021).
Long-term care work is undervalued
Paid long-term care workers often receive low wages, have little job security, suffer from poor working conditions and receive few or no benefits. In the United States of America, for instance, non-residential long-term care workers are paid half of the average national hourly wage (Gould, Sawo, and Banerjee, 2021). Caregivers also tend to be underpaid even in comparison to other occupations whose workers have similar skills, education and experience (England, Budig and Folbre, 2002). Lack of training commensurate with the needs of care recipients can also lead to physical and mental health issues among caregivers and negatively impact the quality of care received by older persons. Although providing care to a family member may have some positive aspects, including the personal satisfaction of helping a loved one, unpaid family caregivers often experience similar mental and physical stress as paid care workers. This can be especially challenging for older caregivers, such as those caring for a spouse. Moreover, family caregivers often have multiple responsibilities, including caring for dependent children, managing household chores and finances, and sometimes also for income-generating activities. Caregivers who are overworked are at risk of providing poor-quality care (United Nations, 2018). Shortages of caregivers and quality care services reflect or poor strategic policy planning or meaningful consultations with older persons as those most affected by such policies. In fact, many countries across different regions lack a specific policy or strategic framework for long-term care. Even in countries with care provision policies, poor implementation has often left older persons, especially the most vulnerable, with fragmented, confusing and inadequate care options. It has also left caregivers with little income security. For instance, lack of legislation on labour standards has left care workers without guarantees on minimum daily and weekly hours, and with limited employment protection or assistance in case of unemployment. As societies age, pressure grows to ensure the provision and affordability of long-term care services for all people in need, which requires investment to keep pace. However, at the global level, average public expenditure for long-term care is stagnating. OECD countries, for instance, spent an average of 1.5 per cent of their GDP on long-term care in 2019, down from 1.7 per cent in 2017 (OECD, 2021).
Care and support systems must be person-centred
Care and support systems for older persons should be tailored to the needs, values and preferences of care recipients and caregivers. They should go beyond the medical aspects of care, encompassing an individual’s culture, life history, social support network and identity, and giving recipients control over care decisions. It should also be holistic, operating across governments, businesses, communities and households, addressing needs for the provision of both paid, formal care and informal, unpaid care. This can improve care outcomes and enhance the wellbeing of caregivers. Such an approach requires investing in both paid, formal long-term care infrastructure and supporting decent work options, including by enabling transitions from informal and unpaid to formal care provision. New legislation—consistent with international labour standards—is needed in many countries to recognize and protect care workers and address inequalities in working conditions; particularly the many women, migrants and members of ethnic minorities over-represented in the care sector. It would also help to improve the domestic supply of care workers by making it a more attractive employment proposition. Countries could also consider adopting migration policies that allow quality, skilled care workers to migrate from other countries through regular channels, when domestic supply is insufficient, while ensuring their rights are protected in the host countries. Making migration partnerships mutually beneficial also requires efforts to build skills and talent within countries of origin, to be deployed domestically, consistent with Objective 18 of the Global Compact for Safe, Orderly and Regular Migration. Countries can also provide more support for people to age in place, retaining family and other social connections. Better support to unpaid family providers of long-term care can help. Providing quality training for caregivers as well as encouraging the use of new technology, such as remote telecare, is important. Extending paid leave entitlements and flexible working arrangements for family care givers enables older people to remain at home and reduce the need for more expensive residential care. These changes may also challenge gender norms about caregiving, by recognizing the inherent value of unpaid care work. Target 5.4 of the Sustainable Development Goals urges recognizing unpaid care and domestic work, providing public services, infrastructure and social protection policies, and promoting shared responsibility for care at the household level (United Nations, 2015). Formalizing care work can contribute to employment and create further opportunities for women to participate in the economy. Finally, better oversight and regulation of care facilities can help address inequalities in care provision. As shown during the Covid-19 crisis, many long-term care facilities are of poor quality and leave residents vulnerable to disease. Governments and private providers should work together to enhance pandemic preparedness, protect the mental health of workers at care facilities and ensure workers are given quality training sensitive to the needs of older persons (United Nations, 2020). Brief-The-Impact-of-COVID-19-on-Older-Persons.pdf
 Welcome to the United Nations
Welcome to the United Nations